Washington University laryngologist Matt Rohlfing, MD, brings new hope to patients with airway deficiencies that are unresponsive to endoscopic management.
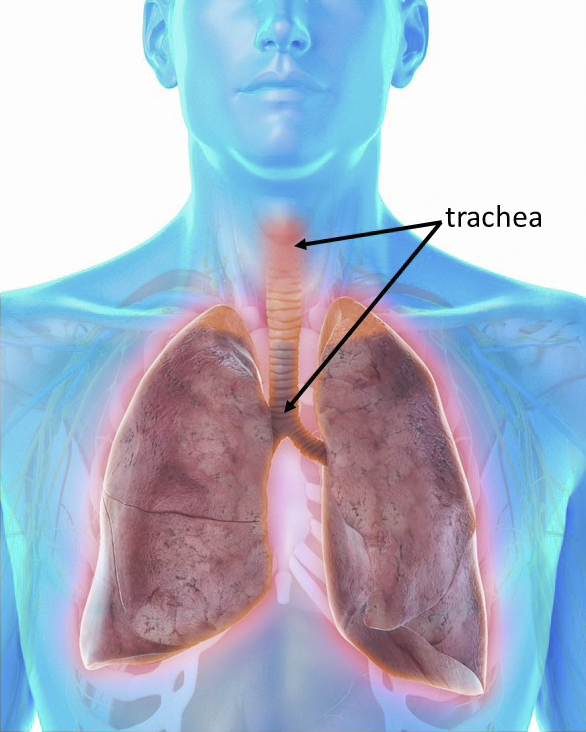
Tracheal stenosis is a narrowing of the windpipe (trachea) that can lead to shortness of breath and coughing. The condition is most commonly caused by trauma due to intubation or tracheostomy – an opening to the airway created from outside the neck. Prolonged intubation and excessive cuff pressure are particularly prone to cause tissue damage that leads to the buildup of scar tissue and subsequent narrowing.
Many cases can be managed endoscopically, typically by gentle dilation of the affected trachea. However, some cases of stenosis – scar which recurs quickly or instability of the tracheal framework – are better managed by removal of the diseased trachea.
For these patients, a tracheal resection is now the preferred option. In this procedure the diseased portion is removed and the two ends attached. According to Rohlfing, about one-third of the trachea can be safely removed with low incidence of complications. Care must be taken to ensure uninterrupted blood supply and avoid damage to the recurrent laryngeal nerve that controls voice production.
“Larger removals do require so-called release procedures to increase the mobility of the distal trachea to allow the cut ends to be approximated,” he said. “The multidisciplinary procedure may require specialists in pulmonology, thoracic surgery and otolaryngology and is one that should only be conducted at a major tertiary center like WashU.”
Sometimes, stenosis leads to a loss of support from the cartilaginous rings anteriorly, resulting in an inward collapse of the lateral tracheal walls, a condition known as A-frame deformity. These cases can be difficult to intubate and are therefore best managed by tracheal resection.
Post-operative care includes special precautions to avoid neck extension that would place tension on the tracheal anastomosis. Respiratory therapists and speech language pathologists specialized in speech and swallowing become important parts of the care team during recovery.
Originally designed as treatment for tracheal stenosis, resection is now widely used for tracheal tumors, trauma, and fistulas.
