For more than 10 years, the mother of two had severe hearing loss. She couldn’t hear her children when they cried, fell, yelled or talked to her.
“It was very depressing and devastating, as it limited my ability as a mother to take care of them,” remembers S. Mahasneh, who lives in Jordan, more than 6,500 miles from St. Louis.
Despite earlier failed attempts to improve her hearing, through surgeries and hearing aids—she was not ready to give up hope. Mahasneh decided to make the trip to St. Louis to see one of the world’s leading neurotologists, Washington University’s Cameron Wick, MD.
The trip more than halfway around the world was worth it, she says.

“I retrieved more than 90% of my natural hearing! I am very happy and impressed by the miraculous job he did. I am back to normal life, with full functionality and no limitations at all!”
Mahasneh’s brother Omar Mahasneh, MD, referred his sister to Wick, because Wick had already helped him with his own ear disease, a chronic ear perforation with drainage.
“Dr. Wick was the fourth ENT physician I saw concerning my ear problem, and the only one who successfully handled it and treated it,” says Mahasneh, who is an internal medicine doctor.
“I wanted a physician who belongs to the new generation with expertise in the new advanced technologies of otologic surgery,” says Mahesneh. And that’s how he found Wick.
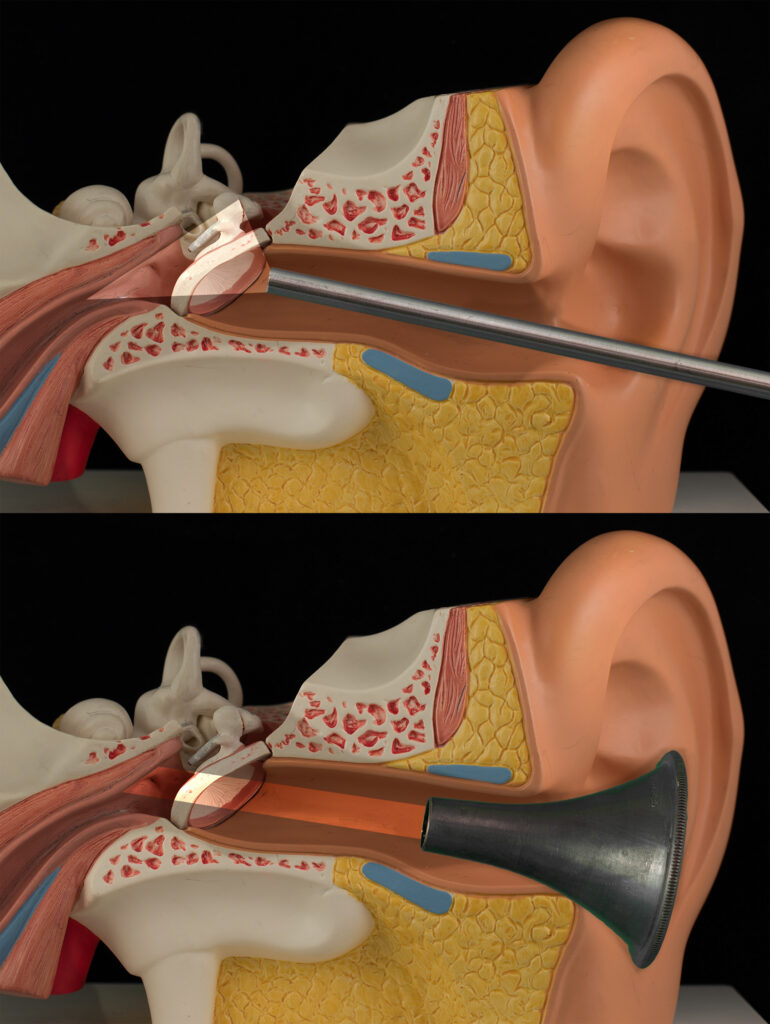
Wick has tools and techniques that many others do not, including minimally invasive endoscopic surgery, which is treating the ear disease by going through the ear canal without having to make an incision behind the ear. This technique, also called transcanal endoscopic ear surgery (TEES), is minimally invasive surgery to operate on tiny, delicate structures within the middle ear, allowing patients to heal faster and have less pain.
Wick would use the endoscopic technique to repair both of Mahasneh’s ear drums and reconstruct the chains of small bones in her middle ear. Both structures are important for transmitting sounds to the inner ear.
Many otologists use the endoscope for the better view it provides but there are still few who use it to conduct TEES or minimally invasive endoscopic surgery, according to Wick. Residents and neurotology fellows at Washington University are now learning these skills in the surgical simulation lab.
Another benefit for international patients seeking treatment from the experts at Washington University School of Medicine is the support of the new International Patient Care office.
By gathering previous medical records, having them translated, and coordinating with the patient care and finance teams prior to the visit, Washington University makes the patient experience simpler, with a real focus on getting the care done as efficiently as possible, according to Phillip Lord, director, International Patient Care at Washington University School of Medicine.
“I am more than happy and satisfied,” says S. Mahasneh, who is back at home in Jordan, finally able to enjoy the chatter, singing and even the crying of her children.
“The experience was pleasant and the outcome exceeded all my expectations,” she says.
Her brother agrees: “Dr. Wick was very generous and welcoming and went above and beyond to help me and my sister more than any other physician I know – including myself as a physician.”
