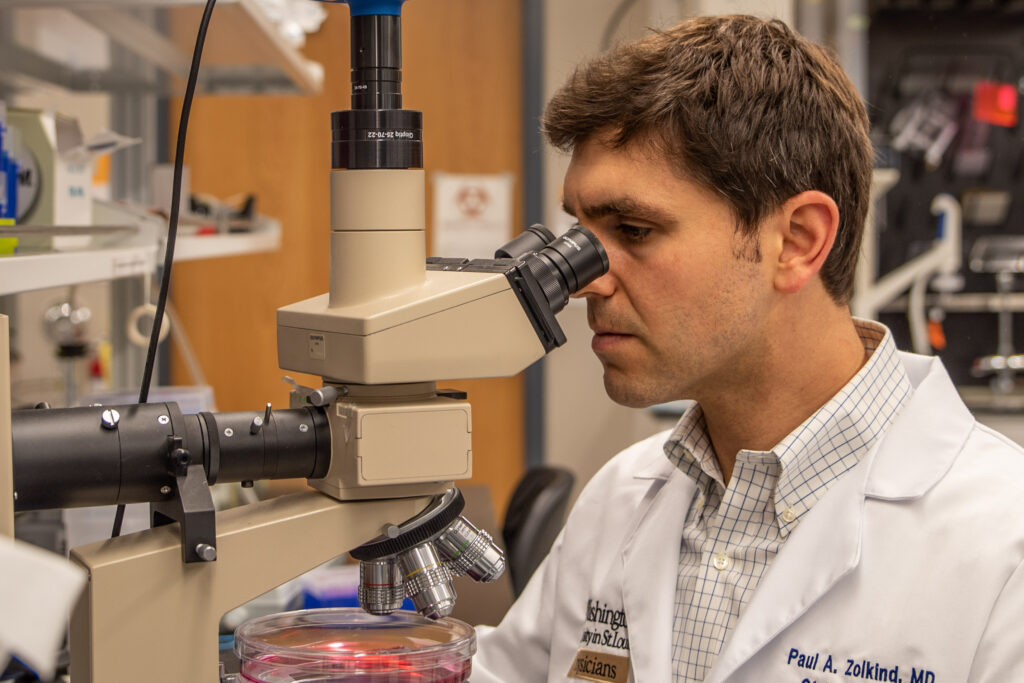
Washington University head and neck surgeon Paul Zolkind, MD, and his collaborators are making great strides in their understanding of why some cancers respond well to radiation therapy and others do not.
One of the most important characterizations of cancers in the past decade is the understanding that no two cancers will progress or respond to treatment in the same way. This has driven the need for a more personalized medicine, or treatments that can be based on the unique genetic and protein signatures of each cancer.
The Zolkind lab is particularly interested in understanding why some head and neck cancers do not respond well to radiation treatment. Radiation is one of the primary treatment modalities for patients with locally advanced disease, but 5-year survival is still a dismal 50%. That may soon change.
The lab recently discovered that activation of the NRF2 oxidative stress pathway is associated with radiation resistance. This pathway is activated in up to 40% of head and neck cancers and is associated with worse outcomes. According to Zolkind, the lab has two primary goals:

- Development of a clinical assay that can provide clinicians and patients with a tumor NRF2 score that can help guide treatment decision making; and
- Development of targeted drugs against the NRF2 pathway that in turn sensitizes tumors to radiation therapy.
Is NRF2 protective or cancer promoting?
NRF2, or nuclear factor 2-related factor is a primary mediator of the cellular response to challenges from reactive oxygen and nitrogen species and other electrophilic compounds and toxins. When left unchallenged, this oxidative stress can lead to the DNA, protein and membrane damage that serve as major contributors to many human diseases, including cancer. However, when present with certain oncogenes – mutated genes that have the capacity to cause cancer – activated NRF2 promotes tumor development and progression.
“Using cell line and animal models, we are working on two therapeutic approaches which potently suppress NRF2 and sensitize tumors to radiation,” said Zolkind. “Understanding how these drugs work and their impact on both the tumor signaling pathways, as well as the tumor immune microenvironment, are current areas of active research.”
Next steps include validating the biomarker assay on a larger cohort of patients to better understand the relative contribution of NRF2 activity compared to standard prognostic biomarkers like tumor size and lymph node metastases. The group is actively seeking to translate their drug discovery efforts into clinical trials.
The lab uses a variety of research tools including CRISPR, a gene modification technique, and live cell imaging, RNA-sequencing and mass spectrometry. Collaborators within the lab and in the Departments of Cell Biology and Radiation Oncology have provided essential expertise and assistance with this project.
Team approach has been the key to success
“Our research is truly a team science approach and benefits greatly from our partnership with Ben Major, PhD, and his lab members Nathan Wamsley and Dhaval Bhatt, PhD,” said Zolkind. “My lab has the tremendous benefit of Postdoctoral Researcher Harit Panda, PhD, and research technician, James Sun. Former lab members Caroline Krall and Natalie Rowland contributed greatly to this work as well.”
For Zolkind, the WashU head and neck cancer research community has been an amazing source of support and collaboration. He acknowledges colleagues in H&N surgery, medical oncology, and radiation oncology for their support, mentorship, and advocacy through the clinical trial and ongoing research.
Zolkind also acknowledges support from The Foundation for Barnes-Jewish Hospital; the Veterans Affairs Office of Research and Development; Siteman Investment Program/Pedal the Cause; and The Washington University Dean’s Scholars Fund.
To learn more, please contact Paul Zolkind.