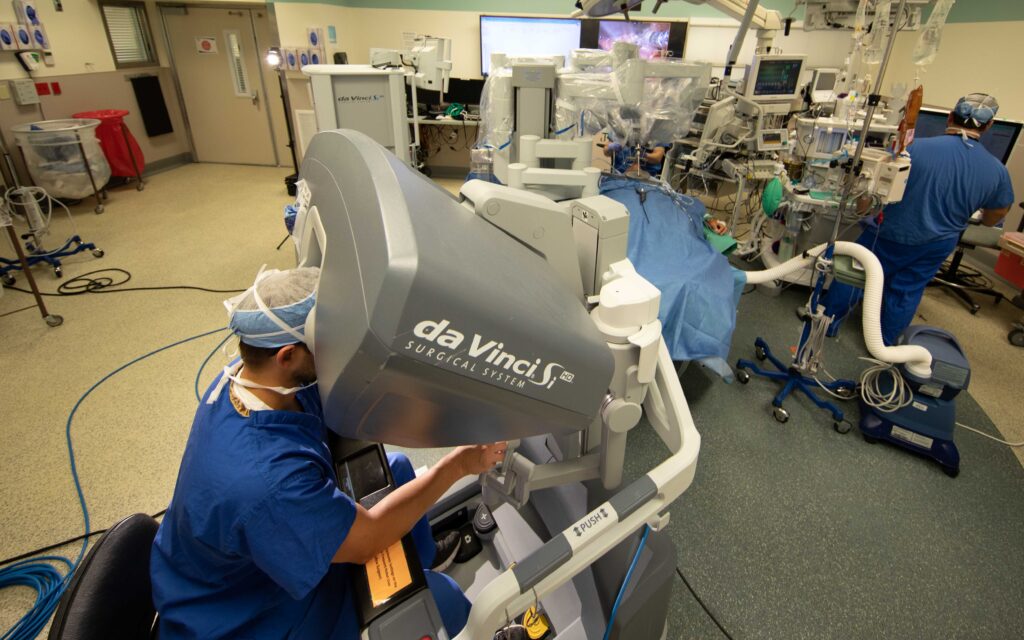
The use of robotic-assisted surgery in the Department of Otolaryngology at Washington University has increased steadily over the past few years, and recent advances in the DaVinci robotics platform should promote even greater usage. Surgeons value the technology for its ability to facilitate difficult surgery through high-resolution 3D visualization, tremor filtration, motion scaling, and a comfortable user interface. Patient benefits include reduced pain and scarring, fewer complications, and reduced length of hospital stay.

National leader in robotic surgery and head and neck surgeon Ryan Jackson, MD, started the department’s robotics program in 2015. Since that time a number of head and neck surgeons have been certified to use the technology, including Randal Paniello, MD, PhD, Jose Zevallos, MD, and Sid Puram, MD, PhD. Dr. Jackson mentors surgeons across the country who are seeking robotics certification.
According to Jackson, the new robot allows the use of two or three working arms with an endoscopic camera system that goes through a single port to access the mouth. This improvement extends the benefits of robotic-assisted surgery by streamlining surgical workflow through the addition of a traction arm.

“The additional arm allows simultaneous dissection and traction,” said Jackson. “As a result we experience better tissue dissection and vessel control. All of our surgeons now exclusively use the new platform.”
Transoral robotic surgery or TORS is now commonly used to remove tumors of the tonsil or base of the tongue. Previous open approaches often required reconstruction, feeding tubes, and tracheotomies, with resultant prolonged hospitalization. TORS achieves the same oncologic outcome with decreased side effects and shorter hospitalization and typically can be performed without a tracheotomy or gastrostomy tube. This has propelled the growth of TORS, largely in HPV-related oropharynx cancers as part of the de-intensification of treatment in those patients.
Dr. Puram started using robotic surgery in 2018 and currently performs two or three cases each month using the new system.
“The robot improves access due to its multiple degrees of freedom and excellent visualization of the tissue,” he explained. “This improves our ability to make oncologic cuts and perform the surgical resection in a way that carefully balances the morbidity of removing normal tissue with a desire to remove a cancer in its entirety.”

Dr. Paniello has also performed robotic surgery for several years now and appreciates the new platform.
“It’s like you’ve miniaturized your hands, and you can really get down into the throat and do the work much more accurately than you could with previous approaches,” he said. “As we get more experience and better instruments, we should be able to do even more with a transoral robotic approach. Traditional transcervical approaches to the larynx, hypopharynx and oropharynx required a partial dismantling of the swallowing apparatus, so avoiding this with a transoral approach would improve swallowing function after these procedures. That would be a big advantage. We are lucky to have Ryan Jackson in our group as a national leader in this work.”