Jay T. Rubinstein, MD, PhD, professor and Virginia Merrill Bloedel chair of the department of Otolaryngology—Head and Neck Surgery at University of Washington Medical Center delivered the 44th annual Senturia Lecture to the Department of Otolaryngology at Washington University School of Medicine on Nov. 13.
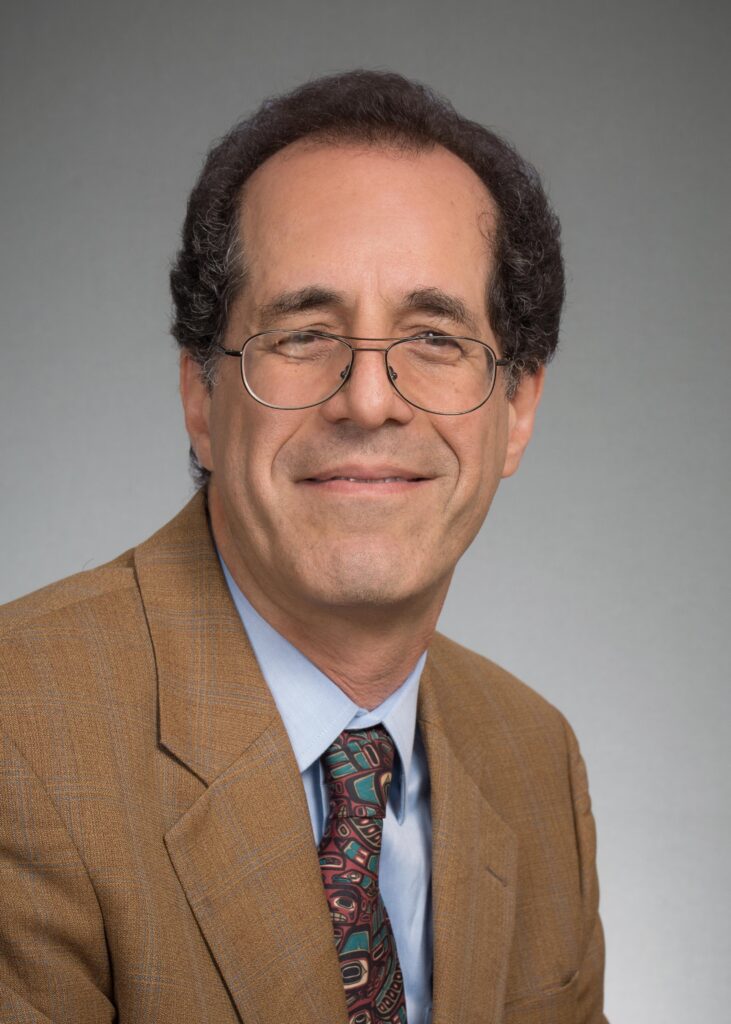
Rubinstein received undergraduate and master’s degrees in engineering at Brown University in 1981/83. He earned his MD and a PhD in bioengineering at the University of Washington in 1988, then completed postdoctoral research training and a residency in otolaryngology at the Massachusetts Eye and Ear Infirmary. He completed a neurotology fellowship at the University of Iowa in 1995, staying as assistant then associate professor of otolaryngology and bioengineering. In 2004 he served as the Boerhaave Professor at Leiden University, the Netherlands.
His talk, “Hearing without a cochlear amplifier: What this tells us about cochlear implants,” highlighted a specific group of patients with a mutation in the gene that produces stereocilin.
In normal hearing patients, stereocilin provides connections between individual stereocilia of outer hair cells in the cochlea and enables their physical association with the tectorial membrane, a structure largely responsible for OHC stimulation following sound-induced movements of cochlear fluids.
Prestin, a motor protein found in the lateral wall, allows stimulated OHCs to resonate at frequencies that can enhance the fine tuning of the cochlea as well as amplify low level sounds, especially those near the threshold of detection. Patients lacking this amplifier exhibit a significant hearing loss, with thresholds about 40 db higher than those with normal hearing.

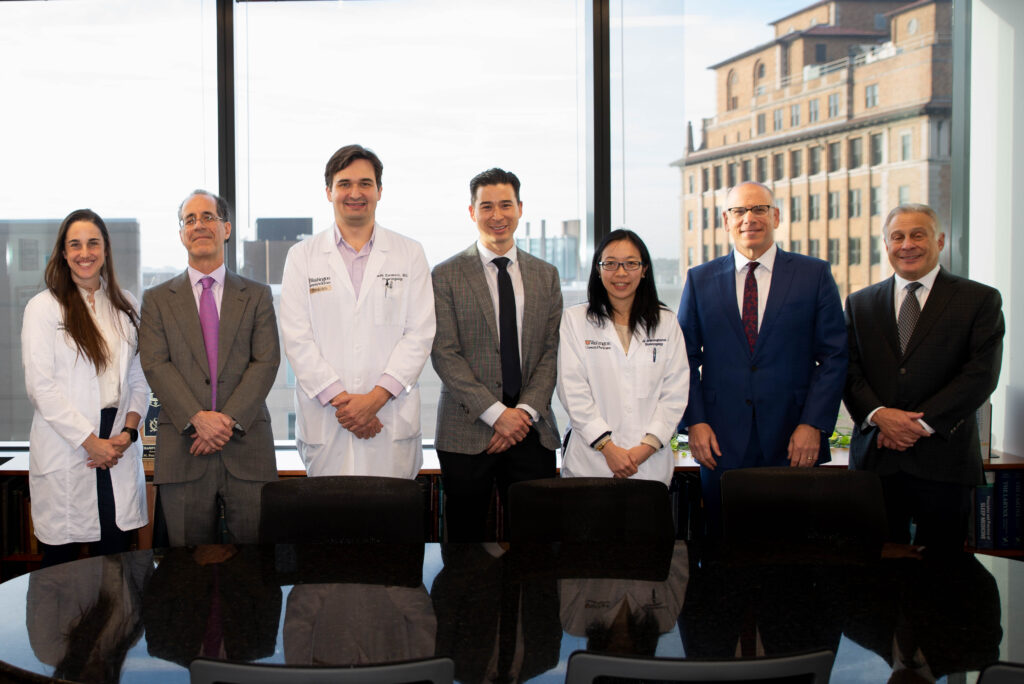
In addition to the lecture, Rubinstein participated in a temporal bone dissection course with senior and chief otolaryngology residents and shared his medical expertise during a review of select case studies presented by residents, Sam Cler, MD, Katherine Garvey, MD, David Lee, MD, and Ruben Ulloa, MD.
The Senturia Lectureship was established in 1977 by the St. Louis Otological Foundation and named for Ben Harlan Senturia, a native of St. Louis who obtained his undergraduate and medical degrees from Washington University. Following his internship and residency at McMillan Hospital, he was appointed to the otolaryngology faculty at Washington University School of Medicine.
According to Division Chief of neurotology Jacques Herzog, MD, Rubinstein’s visit was impactful.
“His participation throughout his visit provided residents, fellows, and faculty with a unique opportunity to learn from a true leader in our field,” said Herzog. “He is well known for his groundbreaking work in both the surgical and scientific aspects of hearing and balance disorders. His lecture was the highlight of the Senturia activites.”