People respond to a crisis in a variety of ways, responses that run the gamut of physical, behavioral, emotional and spiritual reactions. Fortunately, some people respond by looking for innovative ways to help others. Tyler Bertroche, MD, a chief resident in the Department of Otolaryngology at Washington University in St. Louis, is one of those people.

When David Jansen, MD, a med school friend of Dr. Bertroche, returned from travel in Europe he found himself in quarantine, desperately seeking information about his situation. What he found was mostly confusing personal conjecture. To help find real answers, Bertroche, Jansen, and medical school classmates, Kathleen Schroeder, MD, Jessica McIntyre, MD, and Joy Bertroche, MD, formed a Facebook group to collect real-time experiences and research on COVID-19.
To avoid hearsay and conjecture, group members and all posts had to be approved by one of the co-founders. Within days the group had grown to several thousand, and the task of reviewing each post quickly outgrew their capabilities. Twenty additional classmates were recruited to help moderate posts. Within five days, membership in the Facebook group had exceeded 100,000, and it currently exceeds 150,000.
Others began to notice as well. C-SPAN interviewed co-founder Kathleen Schroeder, MD, a family medicine specialist at Northwestern University. And, The New York Times mentioned the group in a feature on the use of social media at the front lines of the pandemic.

One of the primary concerns of many group members was personal protective equipment or PPE, equipment like gloves and masks worn to reduce exposure to hazardous conditions. Among the concerns were availability, proper usage, alternate forms, and adequacy of protection. To help clarify many of these questions, Bertroche distilled the Centers for Disease Control (CDC) and World Health Organization (WHO) recommendations into easy-to-follow guides.
Out of these concerns, new forms of protection started to evolve. An acrylic box used to separate doctor and patient during intubation was tested by Bertroche and some anesthesiology colleagues. When the device proved too restrictive for physicians’ movement during procedures, Bertroche responded with a desire to create something better.
“We wanted to create something that would provide an effective barrier and allow unrestricted movement for the physician,” Bertroche said. “And, it was important that it could be made from readily available materials.”
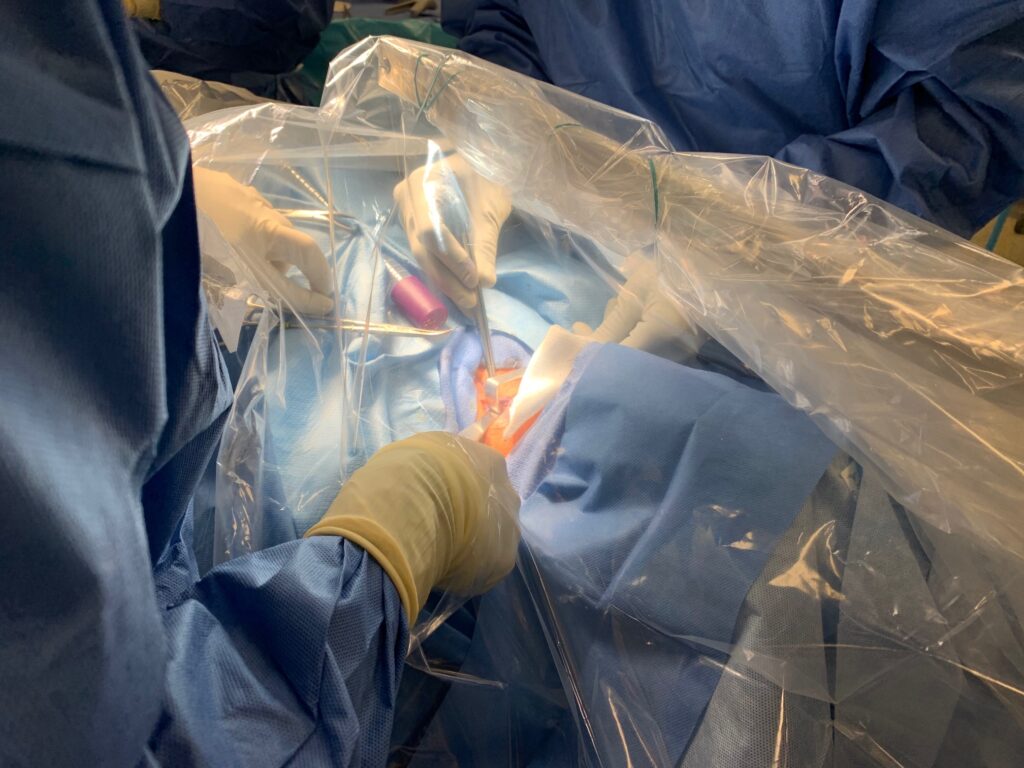
So, with four different materials available at any hardware store, Bertroche created a plastic cover with two arm holes cut and reinforced. Simplicity was key, so it was designed to be assembled in a matter of minutes. Posted to the Facebook page, the idea quickly went viral with an outpouring of support. The aerosol barrier has now been tested in the operating room, and Bertroche is working with anesthesiology and emergency department teams at Washington University School of Medicine to implement the covers throughout Barnes-Jewish Hospital operating rooms.
Bertroche, however, wasn’t done inventing. Another concern all over the world is the shortage of protective masks, so he set about to design and create a reusable N95-style mask that could withstand autoclaving, a form of sterilization that uses high heat and pressure. His choice of material was Halyard 600, the durable blue fabric used to wrap operating room trays for sterilization.

Working with two local seamstresses, a mask was finally designed that passed the N95 fit test to protect the wearer from COVID-19.
“More testing is warranted, but support from the St. Louis sewing community has been tremendous,” says Dr. Bertroche. “We have lots of volunteers lined up to manufacture masks if we can find a safe and effective design.”
“He’s a fantastic leader as a resident, and now also in the COVID-19 space,” said Craig Buchman, MD, chair of the Department of Otolaryngology at Washington University. “And he’s obviously very resourceful. We couldn’t be prouder that he’s on our team.”
Update, April 28, 2020: Manuscript describing the aerosol drape was published in the Journal of the American Medical Association (JAMA) today.
