A delicate surgical procedure conducted by Washington University neurotologist Craig Buchman, MD, offers hope for sound awareness to patients who may not be good candidates for a cochlear implant.
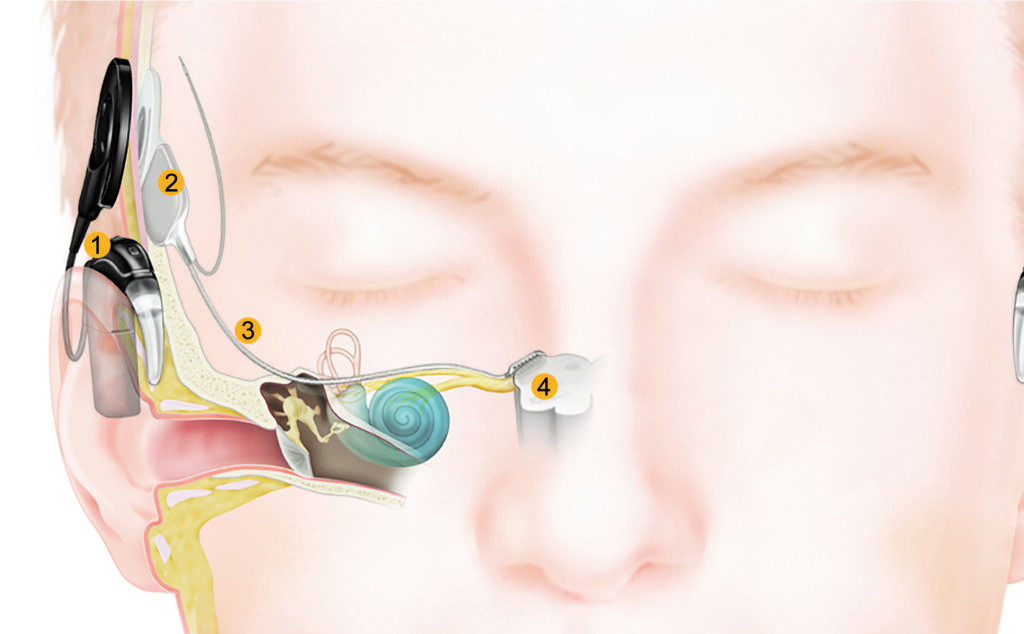
The benefits of the cochlear implant – a device used to stimulate the auditory nerve pathway – are increasingly well known, and the number of devices implanted worldwide is now approaching one million. The device uses a thin string of electrodes inserted into the cochlea that apply small electric impulses to the auditory neurons that transmit information about environmental sounds to the brain.

But, for patients with malformed auditory structures or those with damage to the auditory nerve due to trauma or surgery, the cochlear implant is not an option. For these patients, an auditory brainstem implant or ABI may provide some awareness of environmental sounds.
The ABI works similar to a cochlear implant, but the electrode array is implanted onto the surface of the auditory brainstem, a collection of auditory neurons known as the cochlear nucleus. This allows sound-derived signals to bypass the cochlea and auditory nerve altogether.
Implant designed for NF2 patients
The device was approved by the FDA in 2000 for use in patients with Neurofibromatosis type 2, or NF2. The incidence of NF2 diagnosis is approximately 1 in 25,000, and all NF2 patients will ultimately suffer a profound hearing loss due to the growth of tumors – known as vestibular schwannomas – on their cochlear or vestibular nerves or due to radiation treatments or surgical removal of the tumors.
Buchman now does several brainstem implants each year. For the procedure, he teams with a neurosurgeon and audiologists, who conduct intra-operative monitoring to ensure optimal placement of the electrode array. The procedure typically requires a hospital stay of several days, and recovery period of four to six weeks before the device is activated (turned on).
Outcomes are life-changing
According to Buchman, most implanted NF2 patients achieve some level of phoneme (language sounds) discrimination and environmental sound awareness, but only a small number of recipients acquire true speech discrimination without the use of visual cues.
“Outcomes are rather modest compared to the cochlear implant, though life-changing for the patients,” he said. “Most use the ABI signal together with lip reading or sign language to communicate with others.”
The device is now also being used in non-NF2 patients, including children with malformed or damaged inner ear structures. To learn more about auditory brainstem implants, please visit:
https://oto.wustl.edu/patient-care/ear-hearing/auditory-brainstem-implants/
https://oto.wustl.edu/auditory-brainstem-implant-provides-hope-for-hearing/
