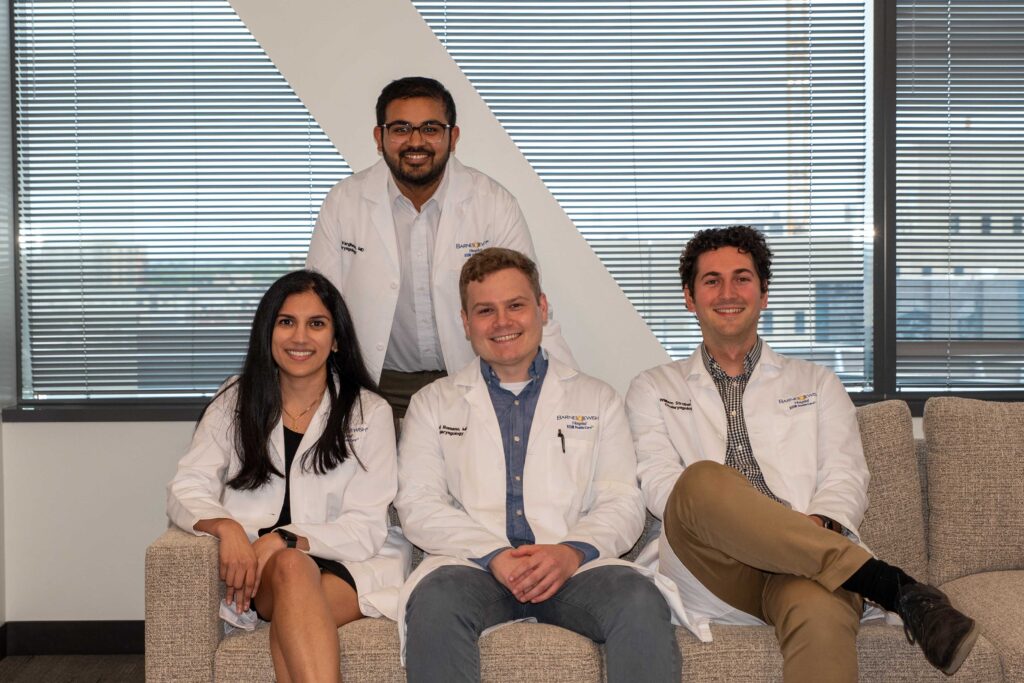
Physician-scientist trainees in the Department of Otolaryngology at Washington University devote two additional years of residency to original research. Four such residents – the first of the new R25 funding mechanism – have chosen their research projects and are aggressively collecting data and seeking answers that will improve patient care worldwide.

Amrita Hari-Raj, MD
Project title: Eustachian tube dysfunction and sinonasal obstruction: A prospective cohort study
Mentors: Jay Piccirillo, MD, Emily Spataro, MD, and Nedim Durakovic, MD
Ear discomfort & nasal obstruction are two extremely common reasons that patients seek otolaryngologic care. Patients with frequent ear popping/pressure/pain often have normal ear exams with no conductive hearing loss, which can make addressing their symptoms challenging. Prior studies have established that symptoms of eustachian tube dysfunction can be associated with nasal obstruction and rhinosinusitis due to turbulent air flow and increased inflammation, and when these patients undergo medical or surgical treatment of their nasal obstruction, their otologic symptoms often improve. This study aims to better delineate this cohort’s characteristics, follow their courses through medical management, identify demographic & prognostic factors of patients who fail medical management, and examine the impact of nasal surgery on treating symptoms of eustachian tube dysfunction. We recently received final IRB approval and are now enrolling patients in the study!
Daniel Romano, MD
Project title: Revealing molecular and cellular drivers of cholesteatoma pathogenesis in children using single-cell RNA sequencing
Mentors: Keiko Hirose, MD, and Sid Puram, MD, PhD
Cholesteatoma is a relatively frequently encountered diagnosis in pediatric ENT and neurotology clinic, with an estimated annual incidence of nearly 1-in-10,000 people. Without surgery, cholesteatoma produces complications such as hearing loss, vertigo, facial nerve injury, and central nervous system infection. The underlying molecular mechanisms of cholesteatoma pathogenesis remain incompletely characterized. Therefore, we are using single-cell RNA sequencing (scRNA-seq) to characterize the inter- and intra-cellular signaling pathways associated with cholesteatoma keratinocyte proliferation, comparing these pathways to those in normal healthy tissue. Validation and optimization experiments for single-cell cholesteatoma dissociation are currently underway in the lab.

Will Strober, MD
Project title: Biofeedback versus laryngeal control therapy in the management of paradoxical vocal fold motion
Mentor: Molly Huston, MD
Paradoxical vocal fold motion (PVFM) is an under-diagnosed and understudied condition that can have major effects on patients’ quality of life. We see and treat it frequently, yet there is little data on how patients respond to different treatments. This is the first randomized controlled trial to study this condition. Our goal is to conduct a pilot randomized study to compare the effectiveness of video biofeedback with behavioral therapy in the treatment of PVFM. The primary endpoint will be the change in Dyspnea Index score before treatment and one month after treatment. Patients will also complete surveys to collate data about expectations of behavioral therapy, their reasons for pursuing additional treatment if applicable, and the perceived benefits of their assigned intervention. We have achieved just under 50% recruitment so far and are continuing to work with patients in the clinics.

Jordan Varghese, MD
Project title: Transtympanic electrocochleography: Preoperatively predicting cochlear implant performance
Mentor: Craig Buchman, MD
Electrocochleography is now being used in the hopes of improving outcomes for cochlear implant recipients. In this study, we propose to evaluate the prognostic impact of transtympanic electrocochleography on postoperative speech perception scores. There have been major strides in using intraoperative electrocochleography to predict cochlear implant outcomes, but there remain several challenges to obtain this information preoperatively. A transtympanic approach is minimally invasive and can be obtained without general anesthesia. We will obtain transtympanic recordings for cochlear implant candidates to build a clinical prediction model for postoperative performance and allow for more informed patient counseling. We are currently troubleshooting recording protocols to develop an auditory evoked setup that is able to meet the strict parameters needed for this research population.