Washington University rhinologist Lauren Roland, MD, MSCI, is leading the charge to improve the prevention and treatment of invasive fungal sinusitis, a rare but aggressive disease with high mortality rates.
About 1 in 7 adults in the US will be affected by sinusitis each year, caused by allergens, irritants, virus, bacteria or fungi. The vast majority of these cases resolve with no complications. In rare cases of fungal sinusitis, the disease invades surrounding tissues like mucosal linings, blood vessels and bone.
Invasive fungal sinusitis or IFS is a rare diagnosis, with only about 15 cases per year at any large hospital. Published mortality rates for IFS are as high as 50-80% due to inadequately defined risk factors and a poor understanding of how non-invasive sinusitis becomes invasive. Roland hopes to better describe risk factors for development of disease to help reduce delays in diagnoses and improve treatment outcomes.
IFS most often affects immunocompromised individuals, such as diabetes patients; transplant recipients; patients undergoing chemotherapy; or patients being treated with one of the many newer immunosuppressive biologic medications. Not surprisingly, the incidence of IFS is increasing as the population of patients on immune compromising medications grows. The emergence of COVID has also raised concern for increased cases of IFS.
Because there are no currently published guidelines for IFS, Roland and colleagues recently conducted a comprehensive evidence-based review with recommendations for diagnosis and treatment of IFS. Some of the principle findings include:
- The relationship of IFS to other forms of fungal sinusitis is unclear, but the risk of progression from non-invasive fungal sinusitis to invasive disease should be a concern, especially in immune compromised patients.
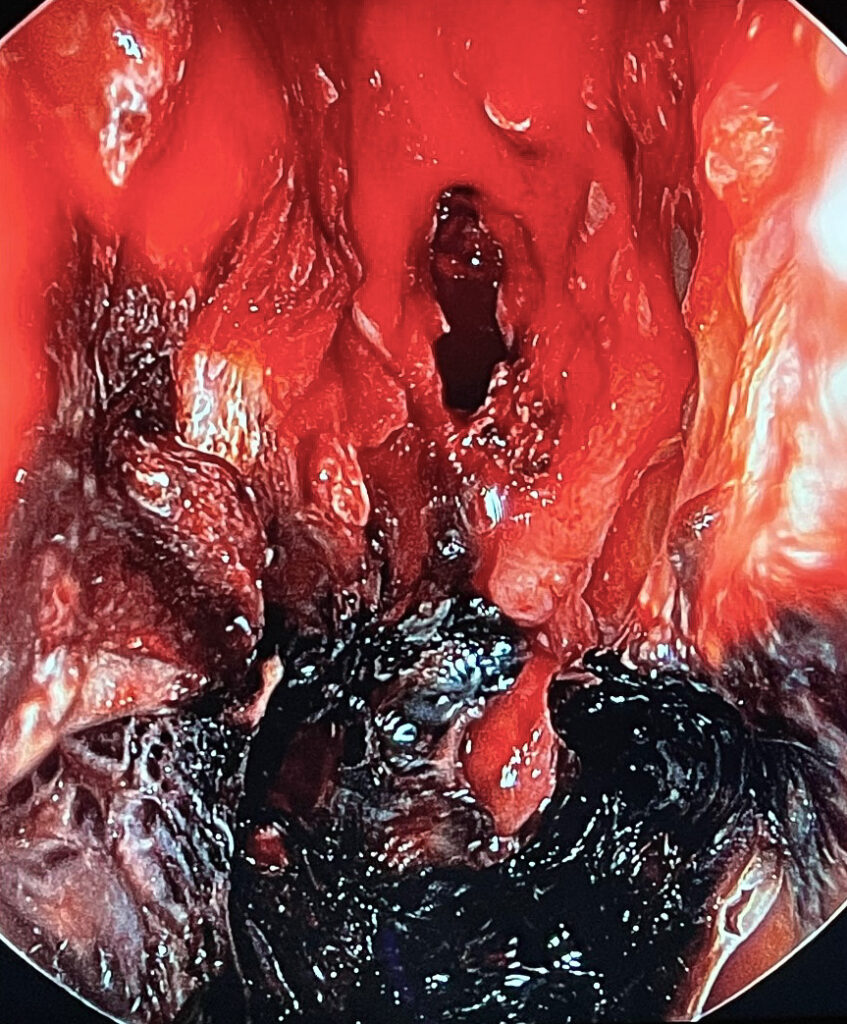
- Criteria for diagnosis of IFS include clinical signs/symptoms, endoscopic exam, biopsy, microbiology testing, histology, and imaging.
- CT and MRI imaging can provide important non-invasive diagnostic tests for IFS.
- Options for management of IFS include surgical debridement, often combined with systemic antifungal therapy.
More research is needed
While Roland acknowledges the review does highlight the highest level evidence for diagnosis, prognosis and treatment of IFS, there is significant room for research and improvement in the management of this disease.
She, along with fellow WashU rhinologists Nyssa Farrell, MD, and John Schneider, MD, and outcomes scientists, recently published a retrospective study evaluating risk factors in bone marrow transplant patients. This was the first study to evaluate risk factors for development of disease in an at-risk population. The study revealed that multiple transplants and previous sinusitis both significantly increased the risk of development of IFS.
Roland has also joined forces with the lab of Peggy Kendall, MD, the division chief of Allergy and Immunology, to study IFS in the laboratory setting.
“We are currently working to build a translational research program to study IFS through blood and sinonasal tissue samples,” said Roland. We are focused on the immunosuppressed population, particularly those undergoing bone marrow transplant for hematologic malignancies.”
Roland was also recently awarded a [KL2] career development award to study the innate immune system’s role in development of IFS using sinonasal tissue and blood from surgical patients.
The study will use immunocytochemistry, mass cytometry (CyTOF) and single cell RNA sequencing to build on recently published work using bulk RNA sequencing on sinonasal tissue in IFS and control populations. The long term goal is to identify cell types or mucosal factors critical for development of disease to help identify preventative therapies.
Another award from the American Rhinologic Society proposes to take this work a step further and will utilize blood from IFS patients over time to evaluate the systemic immune response during recovery from disease. The goal of the study is to immunophenotype cell types associated with survival to help identify novel medical treatments.
To learn more about IFS and ongoing research studies, contact Lauren Roland, MD, MSCI.
