Imagine the feeling of sandpaper dragging across your eyes every time you blink and the inability to produce tears to relieve the pain. This is the suffering that patients with a severe dry eye condition called xerophthalmia often endure. The constant irritation and resultant tissue damage can lead to blindness – unless they’ve found a pioneering head and neck surgeon like Randal Paniello, MD, PhD.
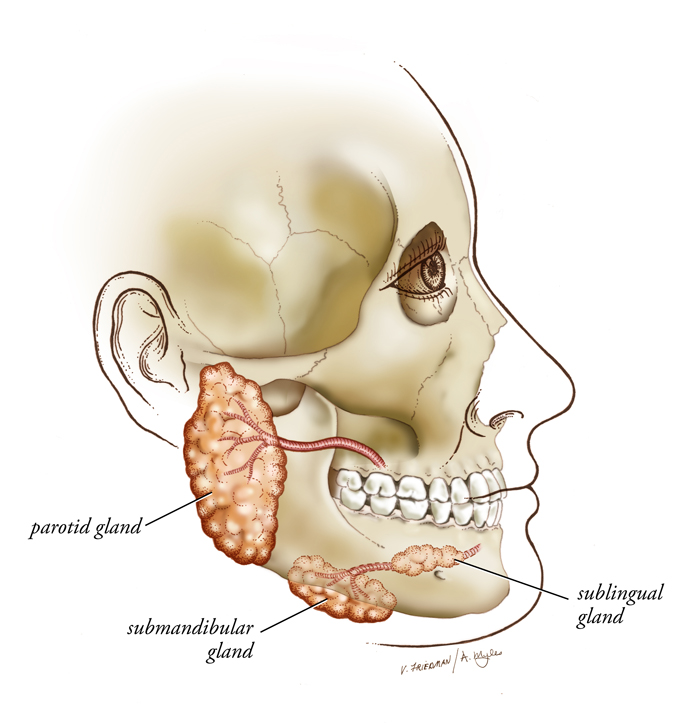
Dr. Paniello was the first in the US to perform a salivary gland transplant to treat xerophthalmia after being challenged by an ophthalmologist colleague to find a solution to this difficult problem. The surgery, which takes approximately six hours, transplants a salivary gland from beneath the jaw to a spot near the temple.
“Traditional treatments include eye drops which have to be applied every 3-5 minutes, or punctal plugs which block the tear ducts that normally drain tears from the surface of the eye,” says Paniello. “The transplant procedure is reserved for the most severely affected patients that have not responded to traditional treatments.”
Since his first ground-breaking surgery in 2005, Paniello has performed the procedure on 15 patients. All of the transplanted glands have survived and produced salivary flow to the eyes, though not all produced optimal amounts of flow. Five transplants produced too much tear flow which ended up running down the patient’s cheek, a condition Paniello calls salivary epiphora.
Creative solutions include using a vein from the leg

Paniello says that reducing tear flow could be easily remedied by removing a portion of the gland, but for those patients needing a similar procedure to also produce tears in the opposite eye, he wondered, why waste it? He chose instead to simply re-route the excess flow to the opposite eye using a portion of the saphenous vein [from the leg] grafted across the forehead. The results were as he hoped – adequate and no longer excessive, tear production for each eye.
Unfortunately, the transplanted glands – like normal salivary glands – can still be subject to duct inflammation and stone development that can impede normal salivary flow. When two of his patients experienced intermittent or reduced flow, Paniello brought in ENT colleague and sialendoscopy expert Allison Ogden, MD, to assist.
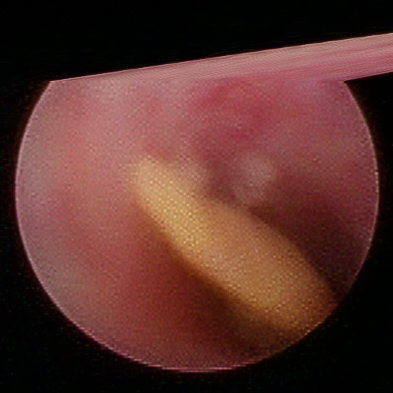
Sialendoscopy is an endoscopic procedure that allows the salivary duct to be examined and cleared, even dilated when necessary. Salivary stones can also be removed during the procedure.
For transplant patients, the tiny endoscope was passed through the conjunctiva, the membrane covering the eye, and into the salivary duct. The duct was cleared of debris, restoring salivary flow to the eye for both patients.
Regaining vision
Clearly the most remarkable outcome has been the return of sight to some patients who had been blinded by their condition. One patient, blind since age seven and who never learned to read, is now being taught to read by his seven-year-old son. Another blind patient, whose condition was caused by an industrial accident, met and married a woman while blind. A few days after his transplant procedure, he was able to see her for the first time.
“Patients who get their vision back are naturally ecstatic about that,” said Paniello.” All patients have been happy with the relief they get.”
The success of the surgery has led Paniello to consider other applications for the procedure. He is currently looking into the possibility of transplanting donated salivary glands for patients with xerostomia (dry mouth). This condition is common in patients following radiation therapy and might offer significant benefit for head and neck cancer patients.
To learn more about the procedure, please contact Dr. Paniello at paniellor@wustl.edu.
