Loss of smell, also known as anosmia, is one of the most common symptoms of COVID-19. The Clinical Outcomes Research Office led by Washington University Professor of Otolaryngology Jay Piccirillo, MD, and Assistant Professor Dorina Kallogjeri, MD, has been conducting olfactory research for the past four years. The lab has investigated several treatments for persistent anosmia (loss of smell), with a special interest in viral-related anosmia.
As the number of total, confirmed COVID-19 cases increases so does the number of people suffering from disease-related anosmia, making anosmia a significant public health problem.

“Our olfactory dysfunction studies in the era of COVID-19 pandemic focus on better diagnosis and recovery of anosmia, development of new tests of anosmia, and different treatment modalities for chronic anosmia, said Dr. Piccirillo. “It is important to note all these studies can be conducted virtually.”
Among several anosmia-related studies the team is conducting or planning to start soon, there are four studies of special interest:
1. COVID-19 olfactory dysfunction study (CODS)
The CODS trial will investigate sensitivity/specificity/likelihood ratio of anosmia as a presenting symptom to the diagnosis of COVID-19, and to explore prevalence and recovery as well as factors predictive of recovery for smell loss.
To determine screening test characteristics of anosmia for COVID-19, we are using a cross-sectional assessment of community-based adults who undergo COVID-19 testing at BJC/WUSM.Subjects will be identified through Epic reports that include: (a) responses to all of the screener questions including responses to the anosmia-specific question and (b) COVID-19 testing results with additional demographic and contact information.
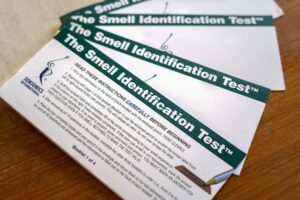
A nested longitudinal study will be used to explore smell recovery among subjects identified with olfactory dysfunction and confirmed COVID-19 diagnosis. Subjects enrolled in the longitudinal study will complete surveys and the objective smell test UPSIT every month until a subject’s UPSIT test is in the normal smell range or for a total of five months.
This study is still open to recruitment. To date, we have successfully enrolled 65 subjects in the longitudinal study.
2. Novel anosmia screening assessment at leisure (NASAL)
The current tests for detecting olfactory dysfunction, including the University of Pennsylvania Smell Identification Test (UPSIT) and the Sniffin’ Sticks, are often time-consuming, costly, and can be culturally specific. Moreover, they can often require a clinician to evaluate the results and are difficult to disseminate widely and quickly in times of need.
The objective of our NASAL study is to elucidate the accuracy of self-reported smell identification of common household items as screening tools for olfactory dysfunction and analyze this data to develop and validate a short smell test using the best-performing household items.
NASAL study will be conducted in two phases. In Development Phase we plan to enroll 120 adults with reported smell changes. Participants will receive access to the NASAL Household Items Survey, in which they will smell a total of 45 possible items commonly found in our households and complete a set of validated surveys together with the UPSIT test. At the end of phase 1, we will create a NASAL Short Smell Test including only the best performing household items for detecting olfactory dysfunction.
In phase 2 of the NASAL study we plan to enroll 200 adults with self-reported smell loss in order to validate the NASAL Short Smell Test. Once developed and validated, this test can be beneficial in not only providing early intervention for older persons who may suffer from neuropsychiatric disease, but also to slow the progression of the pandemic.
Enrollment for the first phase of the NASAL study has recently started and to date there are 10 subjects that have completed this phase.
3. Efficacy of bimodal visual-olfactory training in patients with COVID-19 resultant hyposmia or anosmia using patient-preferred scents (VOLT trial)
VOLT is a Phase 2 Clinical Trial that will evaluate the effects of bimodal visual-olfactory training and patient-preference on olfactory training in patients with post-COVID-19 hyposmia (reduced smell) or anosmia.
We plan to enroll 240 participants and randomize them to olfactory training using four pre-determined scents or four patient-selected scents. Olfactory training typically consists of a patient smelling a scented oil dropped in a labeled jar on a cotton ball for 10 seconds, twice daily, for 12 consecutive weeks. The same participants will also be randomized to either look at a picture representing the odor on a pre-developed study website, or to serve as controls with such no visual intervention.
The specific aims of VOLT trial are:
- Explore the main effects and interaction of bimodal visual-olfactory training and patient-preferred scents in patients receiving olfactory training for hyposmia or anosmia secondary to COVID-19
- Assess the patient-reported, perceived change in olfactory function and health-related quality of life after olfactory training
We just obtained IRB approval for VOLT trial and are ready to start enrollment. If you’d like to participate, please complete our screening survey.
4. Smell in COVID-19 and efficacy of nasal theophylline (SCENT 2)
SCENT-2 is a phase 2 double-blinded clinical trial that builds on previous work completed from the lab. The objective of the trial is to elucidate the efficacy of high-dose intranasal theophylline irrigation in the treatment of COVID-19 related olfactory dysfunction in comparison to placebo saline irrigation.
We plan to enroll 50 subjects. Subjects will be randomized in a 1:1 allocation to the intranasal theophylline irrigation group or the intranasal placebo irrigation group. A member of the research team will instruct participants on how to irrigate each nasal cavity with one-half of the contents of the sinus rinse bottle. Written instructions and a video demonstration will also be provided to ensure proper technique. Irrigations will be performed twice daily – once in the morning and once at night for all subjects. Subjects will be assessed prior to start of intervention, and the 1 week, 3 weeks and 6 weeks after the start of the intervention. The change in UPSIT score will be the primary outcome for the study.
Institutional Review Board (IRB) approval is currently pending for this study.
